ANNAPOLIS, Md. — Paisley Parsons is 10 years into his medical gender-affirming transition, and a majority of that time he’s spent looking for a good team of doctors in Maryland.
Parsons, from near Hagerstown, had limited access to nearby care when starting his transition. Driving to Philadelphia, the District of Columbia or Baltimore were the best options to receive what he needed.
“It took me probably six or seven years to find a team of doctors that I felt like was up to par, but prior to that, finding someone educated and competent was few and far between,” said Parsons. “A lot of it was a proximity issue, and most doctors around me just had no idea about anything trans-related.”
While access to gender-affirming care has improved since Parsons first started his transition, it still varies across Maryland. From finding experienced doctors to the availability of prescribed hormones, trans care can require a lot of work on the patient’s part.
Gender-affirming care is a medically necessary group of treatments, including hormone therapy, alterations to voice, laser treatment and surgeries. But medical “care” also includes using the patient’s preferred pronouns and staying up-to-date on gender identities and protocols.
“Some of my patients travel hours to see me,” said Dr. Helene Hedian, the director of Clinical Education at Johns Hopkins’ Center for Transgender and Gender Expansive Health in Baltimore. “There has been an increased demand for services in the past year, which at times has led to long wait times.”
There is a concentration of qualified doctors in urban areas like D.C. and Baltimore, with less access the farther a patient is from a major city. Geographic centralization of care is not unique to Maryland, according to Hedian, particularly for doctors who provide hormones and surgeries.
Addressing the geographic centralization issue is something the Hopkins Center is working on by providing training to clinicians outside of Baltimore, “but it remains an ongoing challenge everywhere,” said Hedian.
For those looking for a doctor with experience in gender-affirming care, Hedian recommends looking through the provider directory on GLMA: Health Professionals Advancing LGBTQ Equality’s website.
The directory confirms the concentration of doctors in urban areas. For example, a search for gender-affirming hormone therapy in Easton shows the closest doctor is over an hour away in Baltimore, D.C. or Odenton, Maryland.
“Baltimore City is probably the nexus of the trans community in terms of access, but the wait times are really long for our experienced providers,” said Lee Blinder, the executive director of Trans Maryland, a trans-led community organization. “Many people in our more rural areas of the state, or even in some of our counties in our suburban areas, are not able to access an affirming provider.”
Blinder is a founder of Trans Maryland, formerly known as Trans Healthcare MD, which started as a community resource for connecting trans and non-binary residents to qualified practitioners.
“Trans Maryland started out of my own and our other co-founders’ lack of access to gender-affirming care,” said Blinder. “We are extraordinarily lucky to be based in Maryland, certainly looking at the national landscape.”
In May this year, Gov. Wes Moore signed the Trans Health Equity Act, which requires the state’s medical assistance program and Medicaid to provide coverage for gender-affirming care beginning Jan. 1, 2024. Moore also signed an executive order in June, protecting anyone seeking gender-affirming care in Maryland from legal punishment by other states.
“Those two events in the past year have contributed to increased demand for gender care in the state of Maryland,” said Hedian. “People are traveling into the state, especially because in many states they’re not able to receive the care that they used to get.”
As of 2022, 24,000 transgender adults live in Maryland, with an estimated 6,000 enrolled in Medicaid, according to a study by the Williams Institute on Medicaid coverage for gender-affirming care.
The Maryland Department of Health estimated that the number of Medicaid enrollees seeking gender-affirming treatment under the bill would increase by approximately 25 individuals per year, up from 98 in 2022.
Numbers for 2023 are not available, but providers have seen a large increase in the past year.
“We’re aware of the issue and we know that being able to address health care shortages, (is) something that has been long-standing within the state,” Moore said to Capital News Service. “I also know that things like the Trans Health Care Act was the right thing, in the right manner, and we want to make sure that our state is welcoming.”
Moore said that having the medical facilities and personnel to treat people is a priority and that doctor and nursing shortages extend to other areas of medicine.
To adjust to the demand, Dr. Julius Joi Johnson-Weaver, a board-certified family physician, offers gender-affirming care through a program at their private practice. Johnson-Weaver is transgender and non-binary and has experienced many of the care-access issues their patients have dealt with.
It sparks a lot of anxiety, Johnson-Weaver said, when someone is ready to transition “in whatever way it typically starts to feel urgent,” and they are told, “Oh yeah, it’s gonna be six months, you know, or it’s gonna take a long time to get an appointment.”
At the start of Johnson-Weaver’s medical transition, they found that they often had to educate doctors on basic terms related to their care. Often, office staff and doctors would misgender them, making the whole process more uncomfortable. This is common for trans patients.
Trans patients having to educate medical providers about trans people is associated with an increase in depression, anxiety or suicidal thoughts, according to a study done by the University of Michigan and Michigan State University Schools of Social Work. The study also found that over a third of trans and non-binary patients experienced disrespect from providers.
“Seeing specialists as a non-binary trans person, oftentimes, I’m really not able to access an affirming experience,” said Blinder. “I’m providing information, sometimes basically, even what does non-binary mean, and what does that mean for me as a patient within this care.”
These days, trans patients living in major cities have an easier time of finding an experienced doctor. Kerrigan Dougherty, a trans/non-binary Baltimore City resident, had few issues finding qualified care, initially going to Chase Brexton before switching to Hopkins.
“I’ve had a relatively positive experience getting primary care,” said Dougherty. “I’ve been pretty happy with my medical care.”
Dougherty does, however, run into issues with pharmacies not filling prescriptions.
“The pharmacy is the bane of my existence, a never-ending source of stress,” said Dougherty. “Sometimes it’s that my prescription is rejected and other times it is that they say they don’t have the prescription, which doesn’t make sense to me because they can see in my chart that the prescription has been sent.”
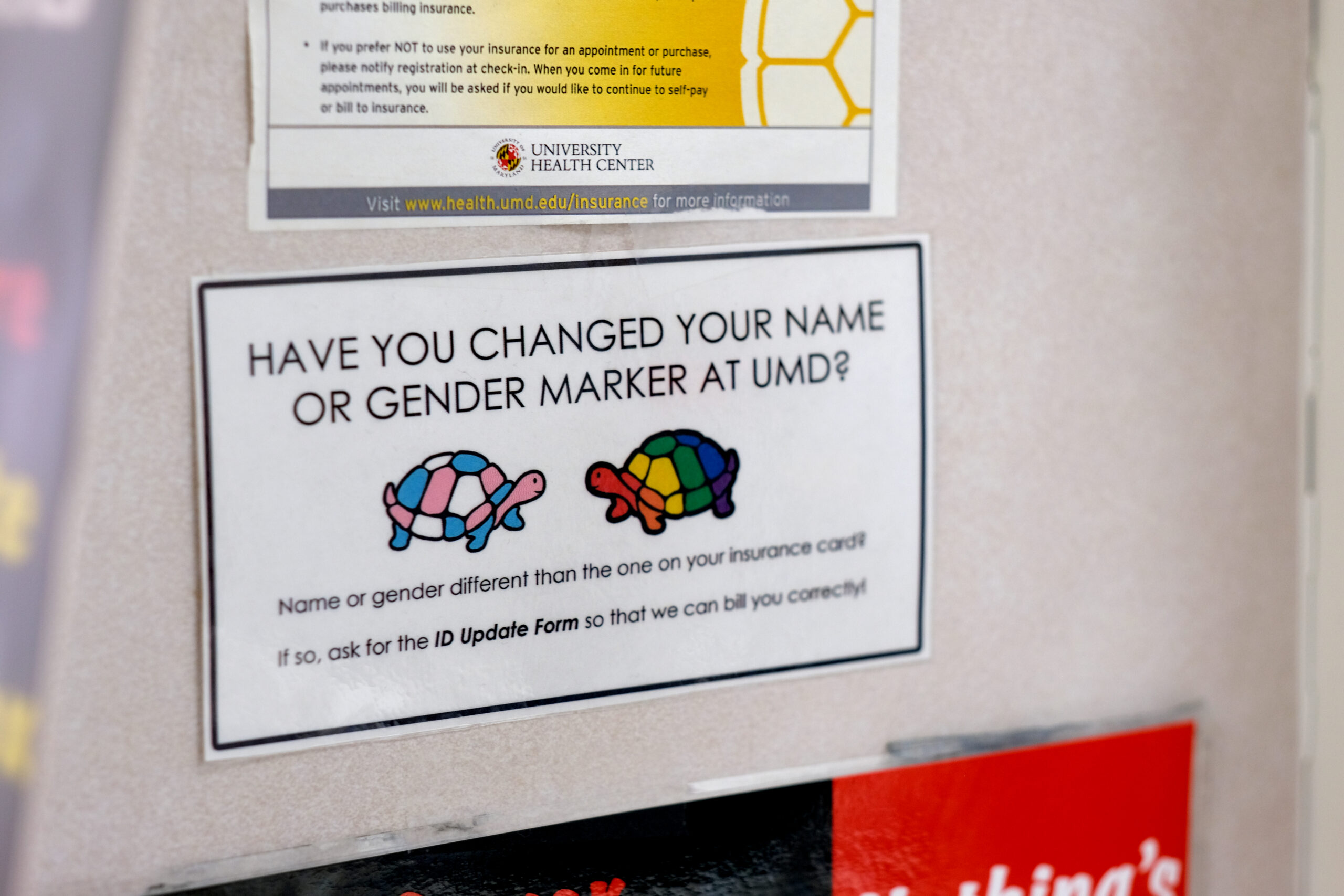
Several factors contribute to trans patients’ pharmacy problems. For one, the insurance classification of a patient’s gender often leads to denied claims.
If the insurer sees that a customer is classified as female, a claim for prescribed testosterone could be rejected automatically, according to Richard DeBenedetto, associate professor at the University of Maryland, Eastern Shore, and a pharmacist specializing in HIV and transgender care.
“Some of the problems with trying to get patients that are transgender their medications have to do with systemic problems,” said DeBenedetto. “Silly as that is – issues with how people are coded on their driver’s license and insurances – to resolve those issues is a legal rigmarole that can take years at times.”
Ongoing drug shortages also contribute to fulfillment problems. In the last two months, the American Society of Health-System Pharmacists reported shortages of the injectable versions of both estrogen and testosterone.
Testosterone is a Drug Enforcement Administration-controlled substance, which limits the amount pharmaceutical companies can manufacture and how much pharmacies can order.
“One manufacturer is not able to just produce more because there’s a need, because another manufacturer can’t, based on the controlled substance regulations,” said DeBenedetto. “This has been a difficult issue to supply people that need hormones for their medications, you know, and you’re kind of hopping around from one to another, trying to make it work.”
Pinpointing what needs to be addressed, whether it’s manufacturers, insurance or health care systems as a whole, is difficult, said DeBenedetto.
“Unless we clearly make decisions that are appropriate, we will continue to run into some issue or another,” said DeBenedetto. “We see lots of transphobia, and until we can really have people seen as people that aren’t any different from anyone else, we’re going to continue to create systems that are classifying people as other.”
Del. Bonnie Cullison, D-Montgomery, vice-chairman of the House Health and Government Operations Committee, cosponsored the Trans Health Equity Act. She said she is aware of the access issues and works closely with Trans Maryland to solve them. And, she said, she agrees with Moore that the bill was the right step for protecting health care for trans-Marylanders.
Trans Maryland was “amazingly supportive” in helping to draft the bill and in helping to answer questions from colleagues,” Cullison said.
Cullison encourages transgender constituents to reach out about these issues: “Talk to us, keep us informed. Let us know what we can do policy-wise or advocacy-wise.”